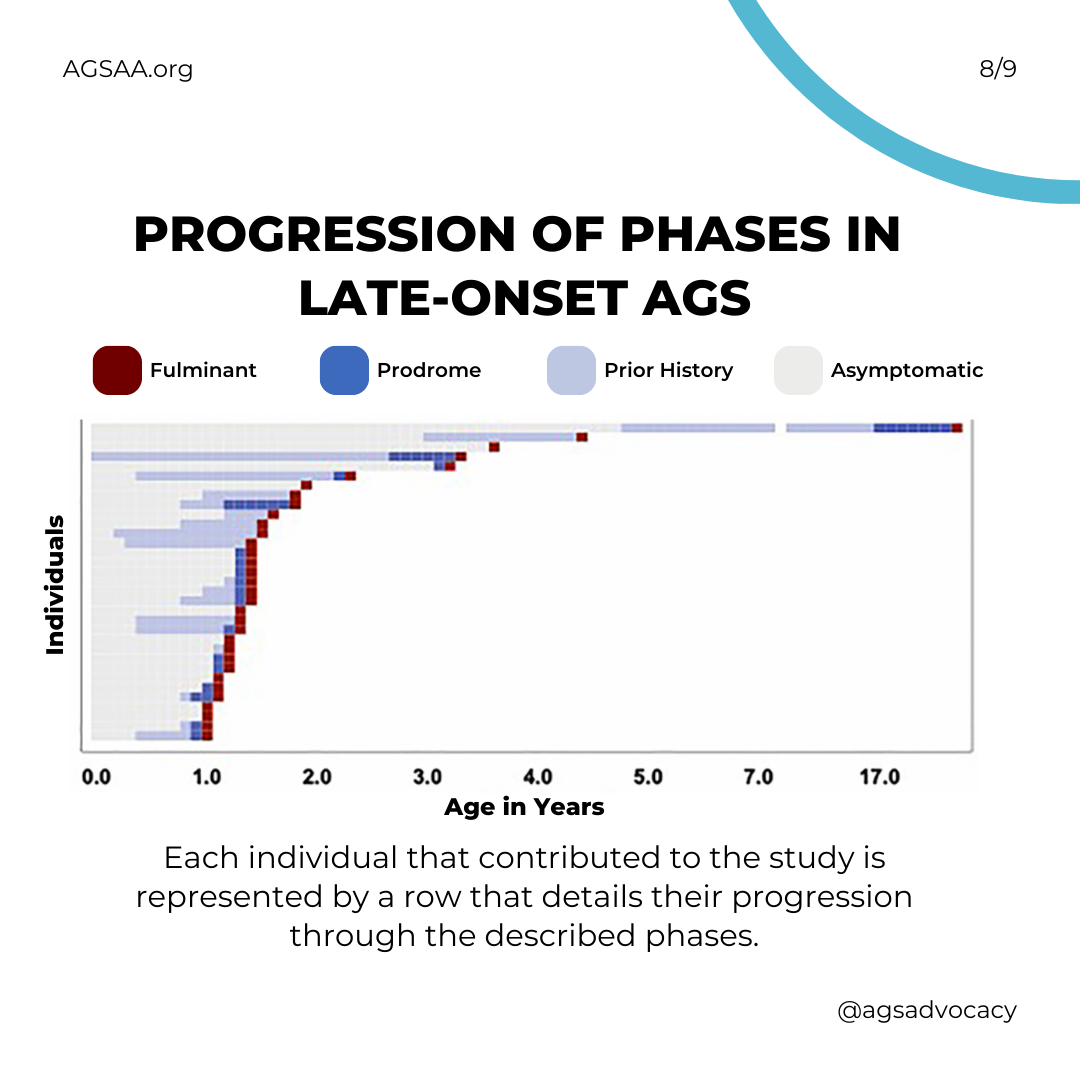
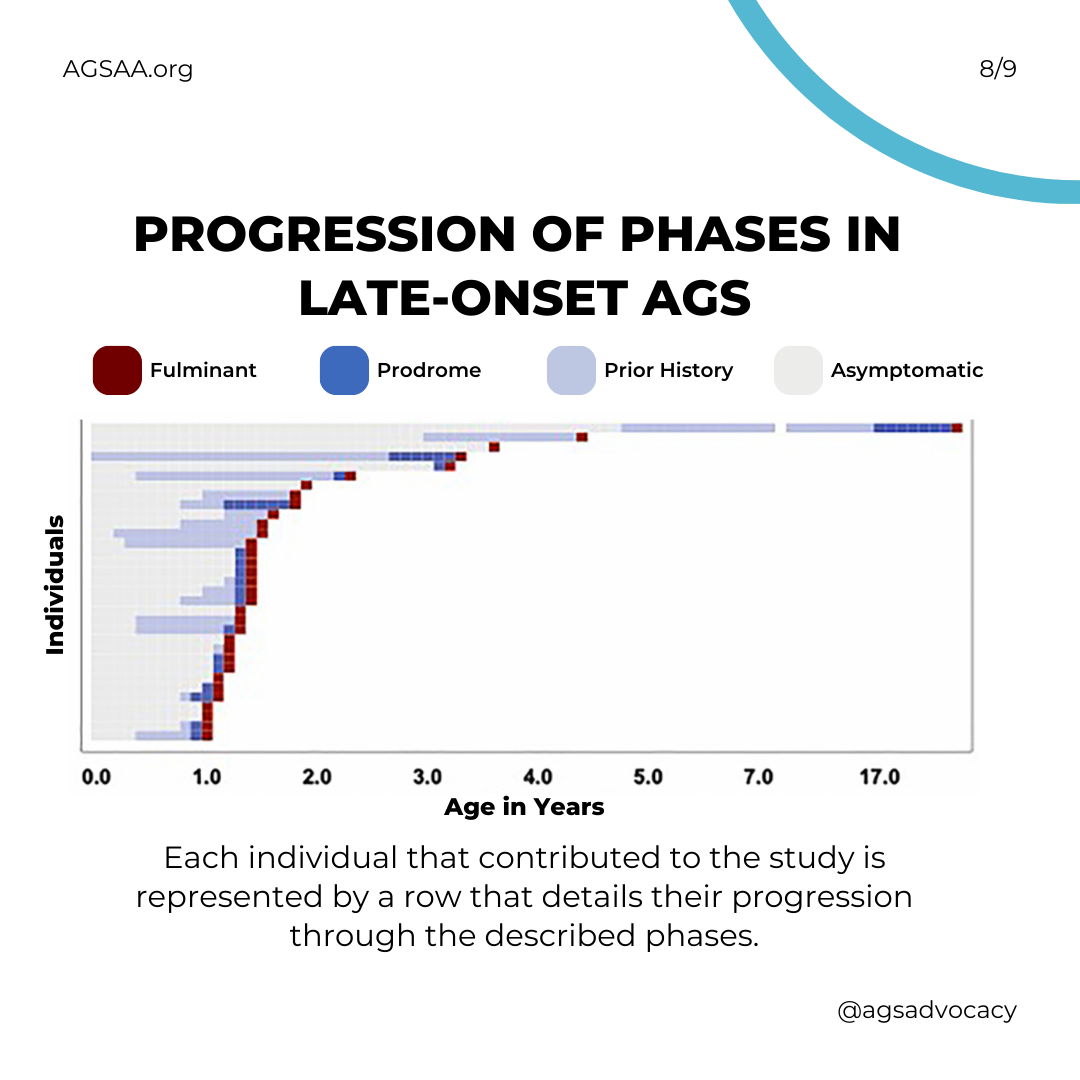
A description of "late-onset" AGS based on 34 children whose disease presented after a year of age.
Late-onset AGS Appears to be More variable
Children with late-onset (aka "atypical") AGS can be different from each other. The clinical course, brain injury, and developmental outcomes of children with late-onset AGS fall on a wider spectrum than that of early infantile onset.
Diagnostic Failures in Atypical AGS Are Common
Diagnosis is complicated by the fact that late-onset children often do not have classical AGS MRI findings (e.g. few have calcifications). While the majority have a medical encounter within a few days of onset, the median time to brain imaging (MRI) is over a month. And, many take over a year to be properly diagnosed. Misdiagnosis is common.
Late-Onset Children Suffer Complications Before Disease Onset
The majority of children with late-onset AGS have a history of AGS-related complications prior to the severe onset of disease. Chilblains, systemic inflammation, irritability, developmental delay and aseptic fevers are common.
Symptoms Worsen Just before AGS HITS
After the early phase, most individuals with atypical AGS demonstrate increasing and worsening features of systemic inflammation during what is called a “prodromal” period. This period typically starts around 1 year and 3 months of age and often includes developmental delay, fevers, irritability, etc.
Then They Crash
AGS causes more severe neurological injury during what is called the "fulminant" phase. This period typically starts about one month after the "prodromal" period and can result in the development of spasticity and dystonia and the loss of gross motor function, vocabulary, and speech.
And Wait For Relief
The length of the "fulminant" phase can vary greatly, but about half of children will have experienced the worst of it within 4 weeks. For a few it fade within one week; while for many others (over one-third) it may continue longer and be considered "chronic."